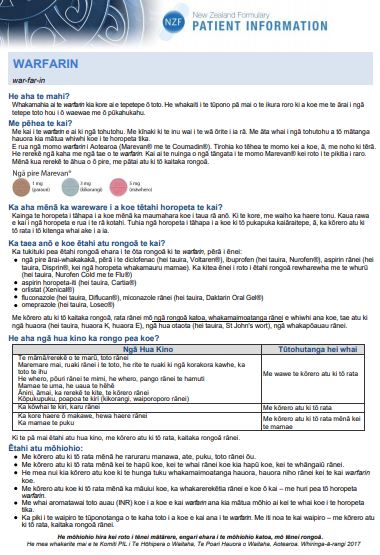
Warfarin shouldn't be taken with some medicines and herbal supplements, so always check with your doctor or pharmacist before starting any new medicines. This includes over-the-counter anti-inflammatories including diclofenac (eg, Voltaren Rapid), ibuprofen (eg, Nurofen) and naproxen (eg, Naprogesic).
Some herbal or 'natural' products (eg, co-enzyme Q10, echinacea, fenugreek, fish oils, dong quai, ginkgo biloba, garlic, ginger, ginseng, glucosamine, kava kava, liquorice and St John’s Wort) are known to have an effect on warfarin. Always check with your doctor or pharmacist before taking vitamins, herbal preparations or dietary supplements.
The commonly prescribed prescription painkiller tramadol may affect your INR results. More frequent testing of your INR is recommended when these two medicines are taken together.
If you're already taking any of these when you're prescribed warfarin, tell your doctor or pharmacist.


 Image credit: NZ Formulary
Image credit: NZ Formulary