Some medicines can increase your risk of falling, especially as you get older and if the medicine makes you drowsy, dizzy, or affects your balance.
Below are some tips on how you can prevent falls when taking medicines.
Talk to your healthcare provider about your fall risk
Older adults may respond to medicines differently and they may become more sensitive to the effects of some medicines. Talk to your healthcare provider to see if any of the medicines you take can increase your risk of falling. Some medicines may cause you to feel faint or dizzy or to experience blurry vision or impaired judgment. Also some medicines can increase your risk of severe injury such as facture or bleeding, after a fall. These are all important side effects to note and discuss with your healthcare provider. In some cases, it may not be a specific medicine causing the side effect – it could be interactions between multiple medicines.
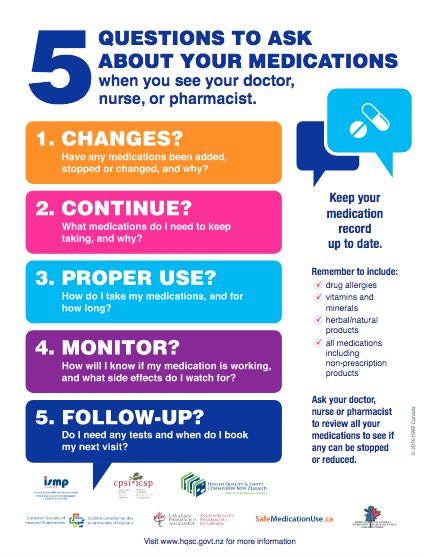
Get your medicines reviewed regularly
If you are taking multiple medicines and you are concerned about the risk of falls associated with the side effects of those medicines, get your medicines reviewed by your healthcare provider. This includes prescriptions, over-the-counter (OTC) and or herbal medicines. Do this at least once a year. Sometimes, under the guidance of your healthcare provider, some medicines can be stopped, or the dose lowered or you can be switched to a safer alternative. If you have had a fall, it is always useful to have your medicines reviewed to prevent further falls.
Be careful when starting a new medicine
When starting a new medicine ask your pharmacist if there any side effects that could put you at a risk of falling. Be careful when you first start a medicine until you know how the medicine affects you. Some side effects like dizziness or drowsiness may be worse when starting a new medicines and may improve as your body gets used to the new medicine.
Get up or stand up slowly
If you notice that your medicine causes dizziness or affects your balance, get up slowly out of bed or stand up slowly. Take a few minutes to sit on your bed or on a chair first. The dizziness should go away after a while. Use extra care if you use a cane, a walker, or crutches.
Check if your medicine interacts with alcohol
It can be dangerous to mix alcohol with some prescriptions, over-the-counter (OTC), or herbal medicines. Drinking alcohol can affect your balance, make you feel sleepy, drowsy or dizzy and it can worsen the side effects of some medicines. Always read the label of your medicine, including OTC and herbal medicines. If your medicine has a warning label to avoid alcohol, then it's best to avoid drinking alcohol while you are taking the medicine. If you are unsure, check with your pharmacist about the effects of alcohol with your medicines. Read more about alcohol and medicines.