Topical steroids are used to reduce inflammation and itchiness in skin conditions such as eczema, dermatitis or psoriasis.
- They are also known as topical corticosteroids, glucocorticosteroids and cortisone.
- Topical steroids work by reducing inflammation which may ease symptoms such as itchiness and redness.
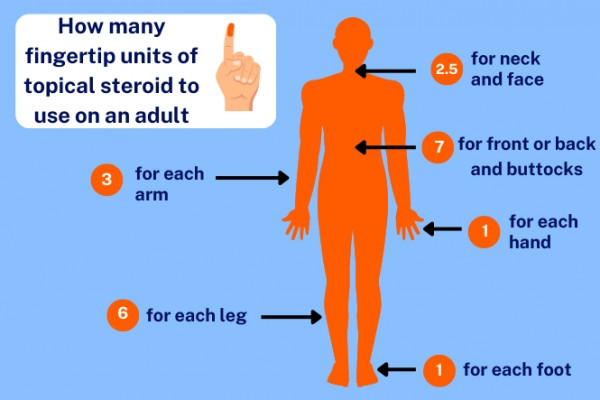
- They are applied to your skin in the form of creams, ointments, lotions or solutions.
- For skin conditions associated with dryness, such as eczema, other treatments such as emollients and moisturisers may also be needed.
- If an emollient and a topical corticosteroid are both prescribed, applying an emollient 20 to 30 minutes before using a topical steroid can help your skin absorb the steroid more effectively.
- Topical steroids should not be used on rosacea or acne.